Pacemakers and AICDs
Pacemakers – trigger heartbeats based on a set rate, some can sense, some can inhibit. Some are dual inhiit and trigger.
Position 1 is where they initiate
Position 2 is where they sense
ICDs – always watching R-R interval, so as to keep an eye on vtach. Either does anti-tachy pacing or shock. Most shocks are from SVT, most ICDs also have antibrady pacing functions.
Think what can be the problems
1. pacemaker gets destroyed
2. it fires when it shouldn’t
3. fails to fire when it should
For example, if it detects bovie as a beat then it might not fire when patient is actually brady. R on T is another problem that can happen. Biventricular pacing can lengthen qt interval, so defib pads essential.
Synchronous vs. Asynchronous
Asynchronous = no sensing, so allow for competitive rythm generation, so electrosurgical stim won’t interfere
3 asynchronous modes
-AOO
-VOO
-DOO
Modern ones not done like this, but good if see one that they won’t have a problem with surgical stim.
Practice Advisory
-if electromagnetic interferencelikely then set to asynchronous mode
-avoid placing magnet on an icd
-pad and bovie should not pass through pulse generator or leads
-use short/irregular lowest energy cautery
-use bipolar or harmonic
-Litho: avoid beam near pulse generator, disable atrial pacing to avoid RonT
-emergency defib: remove magnet ot reenable anti-tachycardia function
Post Op – interrogate and restore
Magnets
-use with extreme caution, you can end up turning off an ICD removing tachydysthr. detection
-most will convert to high rate asynchronous mode (80-100bpm) and less will go to asynchronous mode at a programmed rate or 60-100bpm
-removing magnet –> pacemaker mediated tachycardia from retrograde P waves picked up by dual sensing pacemakers (DDD, VDD), correct by reapplying and removing magnet
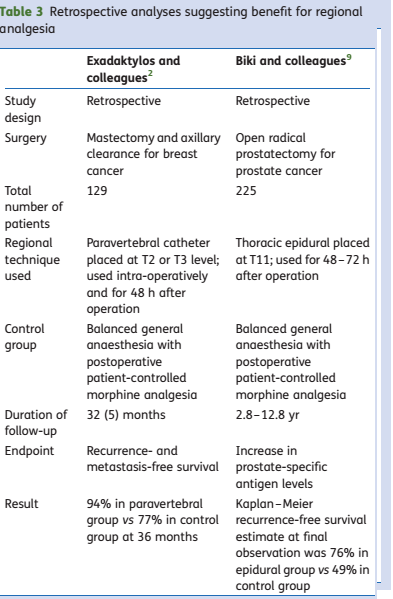
Pacemaking Modes
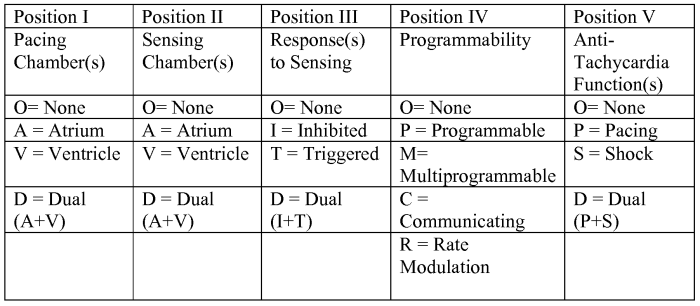
Common modes
DDD
Four rhythms possible
-NSR, Atrial sensed Ventricle paced, atrial paced ventricle sense, atrial + vent pacing
makes sure atrial event –> vent contraction
stops itself if it senses QRS
guarentees atrial kick
VVI
single chamber demand
paces entricle at preset rate(LRI is lower rate interval)
if it senses a ventricular beat it resets clock
prevents RonT
it allows for AV synchrony if atria is passing beat onto ventricle
this pacemaer can lead to pacemaker syndrome if there is loss of AV synchrony and it’s paced ventricle without any atria
Pacemaker Syndrome = fatigue, palpitaions, cough, chest fullness, cannon a waves, elevated venous pressure) and decreased CO… 25% incidence in VVI patients, severe in 5%
Other pacemaker modes
VDD – partially synchronous, pts in NSR but bad AV node. senses atria and triggers ventricle if needed but inhibits if QRS detected, also triggers when pt brady, but cannot cause atria to beat.
DDI – partially synchronous – paces atrium and ventricle at some predetermined rate but can inhibit either based on detection.
VOO – Asynchronous – fixed rate wtih no regard to pt rythm. CAN give RonT
What to do?
Pacemaker Algorithm
1. determine why pt has device, and underlying rythm
2. get a magnet, pads, atropine and isoproteronol
3. interrogate and dtermine voltage / impedence, if >2.6v or 30000, may need to replace before surgery if possible. If ICD has charge time >12s may need battery.
4. Turn off all ICD functions and use pads with EKG
5. Turn off all rate enhacements
6. Turn off minute vent response
7. Consider increasing pacing rate
8. determine magnet function
9. put defib pads on all ICD patients
10. I/O use a-line, ground placement, bipolar cautery, and disable artifact filter on ekg