Carcinoid Tumors and Anesthesia: Notes from TrueLearn
Carcinoid Tumors: Slow growing, benign, small intestine tumors that can metastasize
Hormonal secreting tumors -> cause cutaneous flushing of head neck and thorax, bronchoconstriction, hypotenion, diarrhea, heart disease
Carcinoid Crisis: triggered by physical/chemical such as histamin release, serotonin, bradykinin
Other triggers include: chemo, tumor necrosis, or succinycholine induced fasciculations!
Anesthestic management: avoid histamine release (succ, atracurium, thiopental, morphine, vancomycin); Desflurane good for patients with liver metastasis as low hepatic metabolism (0.02%); Also the use of NE, epi, Dopamine and isoproternol a/w carcinoid crisis
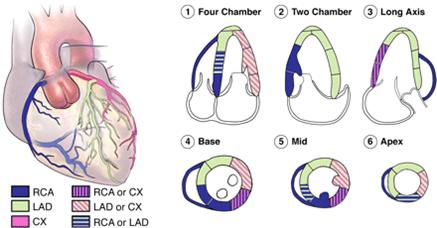
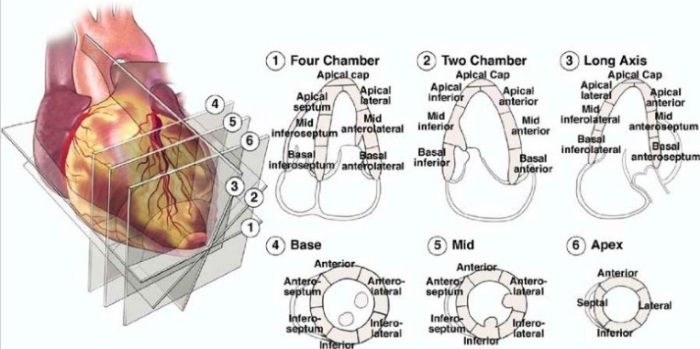
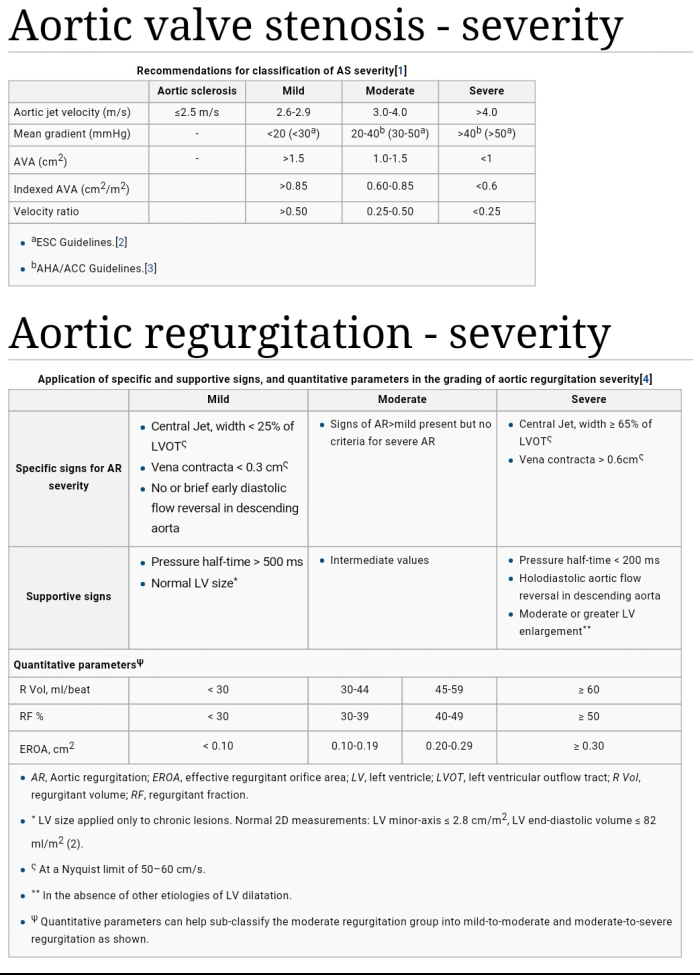
Carcinoid Heart Disease seen in 60% of patients with carcinoid ->right side: tricuspid and pulmonic valves (plaque like deposits on valves) with TR as most common finding; 50% of carcinoid deaths are from cardiac involvement
So Carcinoid Triad = flushing, diarrhea and cardiac involvement
Management I/O And Peri-Op:
Carcinoid tumors secrete variety of substances (serotonin, catecholamines, histamine)
Somatostatin therapy is standard of care
Be prepared for rapid BP changes
-alpha/beta blockers for HTN
-Vaso for hypotension, or neo
Avoid: Beta agonists -> increased release of from carinoid !
https://www.openanesthesia.org/carcinoid_crisis_treatment/